When a loved one is nearing the end of their life, many questions can come up, and quite often, people wonder about medical devices like pacemakers. It's a very natural concern, you know, to think about what happens with these devices as someone approaches their final moments. People often ask whether a pacemaker needs to be switched off when someone is dying, and that's a really important thing to talk about.
This article aims to shed some light on a topic that can feel a bit heavy: how does a pacemaker work when someone is dying? We'll explore what these devices actually do, and perhaps more importantly, what they don't do, especially during life's last stages. It's about finding some clarity and peace of mind during a very sensitive time, really.
We will walk through the common misunderstandings and provide information to help you understand the role of a pacemaker at the very end of life. It's important to have this knowledge, so you can, like, feel more prepared and less worried about these medical aspects.
Table of Contents
- Pacemakers and the End of Life: What You Should Know
- Why a Pacemaker Does Not Prevent Death
- Pacemakers Versus Defibrillators: A Key Difference
- The Option of Deactivating a Pacemaker
- What Happens to a Pacemaker After Death?
- Frequently Asked Questions
Pacemakers and the End of Life: What You Should Know
A pacemaker is a small device placed under the skin, often near the collarbone, to help regulate a person's heart rhythm. It sends out electrical pulses to make the heart beat at a steady rate, especially if the heart's natural rhythm is too slow or irregular. For many people, these devices bring a lot of good years, helping them live a more normal life. But, you know, the question often comes up about what happens with such a device as someone approaches the very end of their life.
It's important to understand that a pacemaker, while a truly helpful medical tool, is not a device that can keep someone alive indefinitely, especially when other bodily systems are failing. People often make assumptions that pacemakers prolong the dying process and thus prolong suffering, but this is usually not the case. In fact, a pacemaker is not a resuscitative device at all, so it's not meant to bring someone back from a complete shutdown, as a matter of fact.
When we talk about how does a pacemaker work when someone is dying, it's about recognizing the device's true role. It supports a heart that's struggling with its rhythm, but it cannot fix all the other problems that might lead to someone's passing. This distinction is pretty important for families to grasp, as it can ease some worries about artificial prolongation, you know.
Why a Pacemaker Does Not Prevent Death
One of the most common misunderstandings is the idea that a pacemaker can somehow prevent death or artificially keep the heart beating after someone has passed away. This is simply not what happens, actually. If the heart stops functioning due to other reasons, such as a lack of oxygen or a complete cessation of electrical activity, the pacemaker will no longer be effective, and the heart will stop. So, the pacemaker does not prevent death or artificially keep the heart beating after someone passes away, you see.
When the Heart Stops for Other Reasons
Think about it like this: a pacemaker helps the heart beat correctly, but it can't make the heart muscle work if it's starved of oxygen. Once someone stops breathing, their body can no longer get oxygen, and the heart muscle will die and stop beating, even with a pacemaker. Therefore, the pacemaker will not prevent death, and a patient will die from their terminal illness without turning off the pacemaker, that's just how it works.
Most dying patients, it's been observed, become acidotic before cardiac arrest. This change in the body's chemistry makes the pacemaker effectively nonfunctional, as under such conditions, the heart muscle does not respond to the pacemaker's discharges. So, for most patients, an active pacemaker will not affect the timing or circumstances of death, which is something to consider.
Terminal events, the medical reasons someone is dying, are often due to things like widespread infection, severe bleeding, blood clots in the lungs, or heart rhythm problems that come from metabolic imbalances. These are big, systemic issues that a pacemaker simply isn't designed to address. It's like, the device is for rhythm, not for total body failure, you know.
Acidosis and Pacemaker Function
The body's chemistry changes quite a bit as someone nears the end of their life, and one of these changes is often a buildup of acid, a condition called acidosis. This acidic environment has a pretty significant effect on the heart muscle. It makes the heart less responsive to electrical signals, including those sent by a pacemaker. So, even if the pacemaker is sending out its little electrical nudges, the heart muscle might just not react to them, really.
This means that, in most cases, as a person's body begins to shut down, the pacemaker's ability to influence the heart's beating diminishes naturally. It's not that the pacemaker stops working, but rather the heart itself becomes unable to respond to its commands. This is a key reason why a pacemaker typically won't prolong the dying process, as a matter of fact, even if it's still technically "on."
This natural process helps to explain why families don't usually need to worry about the pacemaker artificially extending suffering. The body's own changes make the device less and less relevant to the actual timing of passing. It's a subtle but important point, so it's worth understanding, you know.
Pacemakers Versus Defibrillators: A Key Difference
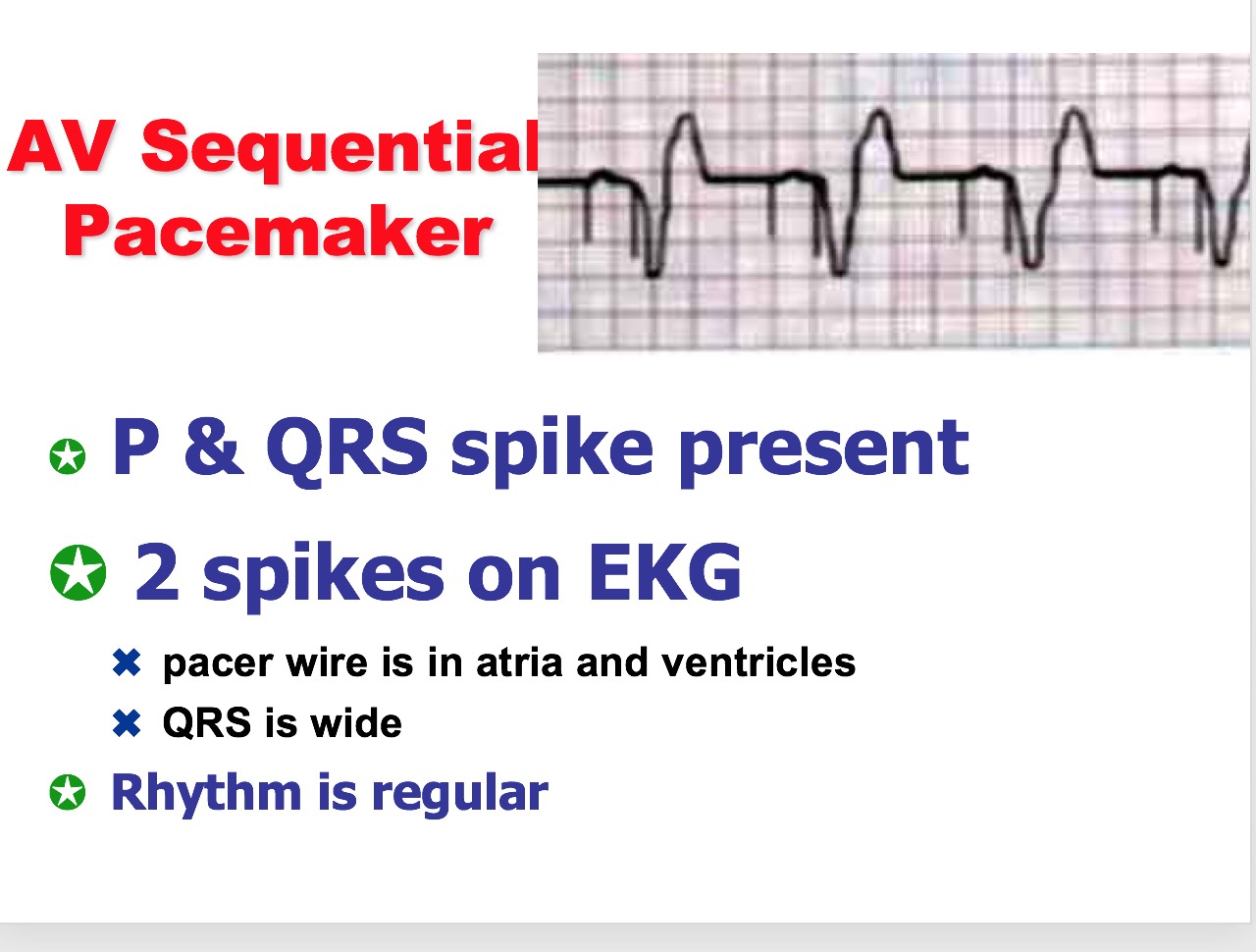
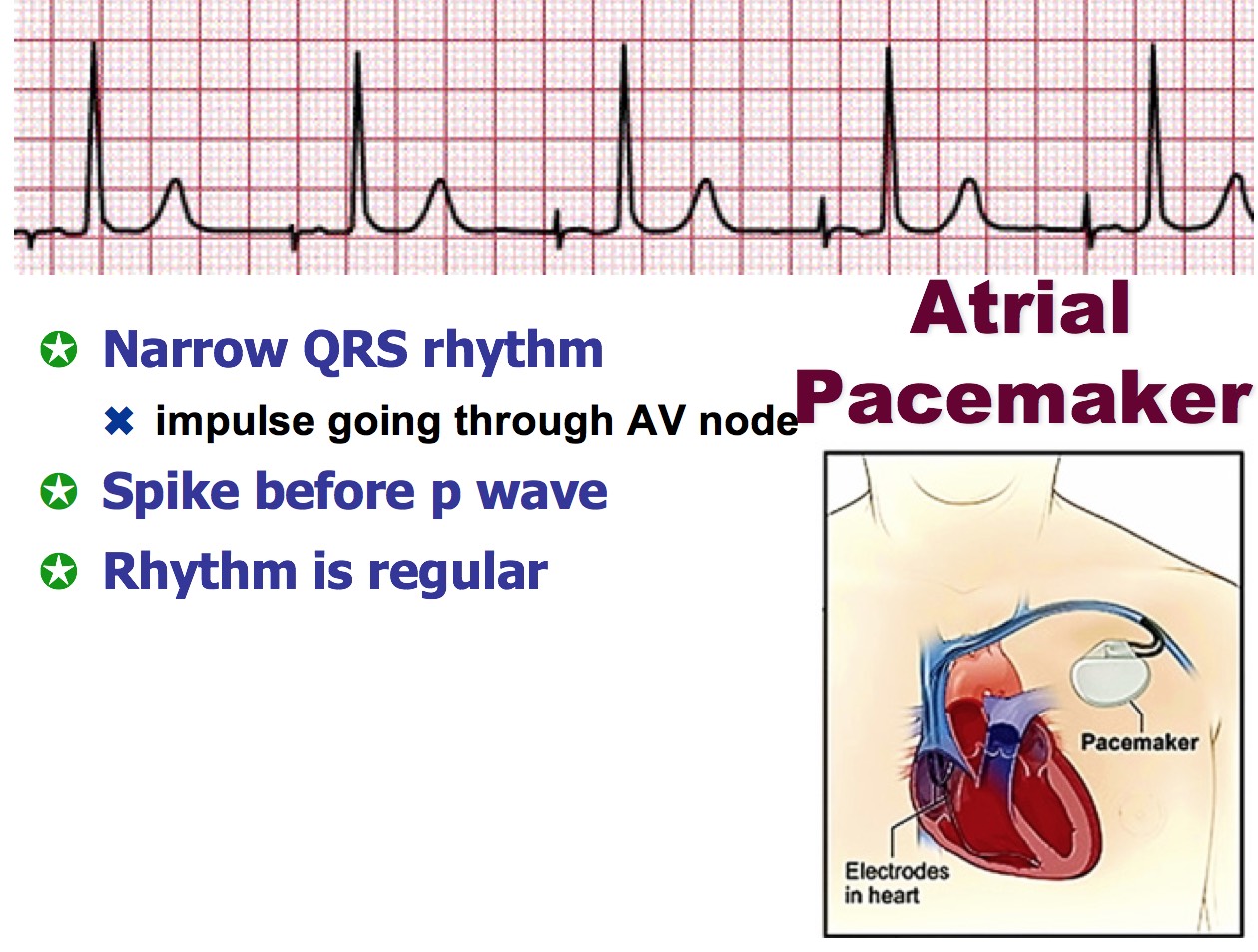
It's very, very important to know the difference between a pacemaker and an implanted defibrillator, sometimes called an ICD. While both are cardiac devices, they do very different things, especially at the end of life. A pacemaker, as we've talked about, helps maintain a steady heart rhythm, basically. It sends out small, regular electrical pulses if the heart's own rhythm is too slow or irregular, you see.
An ICD, on the other hand, is designed to deliver a much stronger electrical shock to the heart if it goes into a dangerously fast or chaotic rhythm. These devices can truly save lives by shocking a heart beating wildly out of sync back to a regular rhythm. But, and this is a big "but," they can also make a dying patient's last hours agonizing, delivering shocks that are meant to restart the heart, but which can be incredibly painful when someone is already very frail, you know.
This is why there is an immense difference between turning off ICD shocks and turning off a pacemaker. Cardiac pacing, unlike ICD shocks, does not burden the dying patient. A pacemaker just keeps trying to pace, which isn't painful, whereas an ICD shock is a jolt, a big one. So, while families often consider deactivating ICDs to prevent suffering, deactivating a pacemaker is a different conversation entirely, often not as urgent for comfort reasons, you know.
For someone with an ICD who is dying, the decision to deactivate the shock function is often a very compassionate one, aimed at ensuring a dignified death. It may, therefore, become necessary to deactivate a patient’s ICD, or, where a device acts as both a pacemaker and a defibrillator, only the element of the device that administers the shock. This distinction is crucial for patient comfort at end of life, actually.
The Option of Deactivating a Pacemaker
While a pacemaker typically does not prolong the dying process, some patients or their families still choose to have the device deactivated. This choice often comes from a desire for a more natural death or a hope for an easier or earlier passing. It's a deeply personal decision, and it's something that can be discussed with medical professionals, too it's almost a common thing now, you know.
People often ask whether a pacemaker needs to be switched off when someone is dying, and the answer is that it's a choice, not a requirement for most situations. If the decision is made to turn devices off, a cardiologist or a pacemaker company representative, who usually has someone on call 24/7, may perform the procedure. This case asks whether a pacemaker can be deactivated to prevent unnecessary prolongation of life, and the answer is yes, it can be, in a way.
Patient Rights and Choices
Every person has the right to refuse medical interventions or to request their withdrawal. This includes devices like pacemakers. This right is a very important part of patient autonomy, allowing individuals and their families to make choices that align with their values and wishes for end-of-life care. More patients (or their surrogates) are requesting the deactivation of cardiac devices at end of life, which is a trend we are seeing, you know.
For those with advanced heart disease or dementia, for example, the conversation around deactivating an AICD (automatic implantable cardioverter-defibrillator) may prevent painful shocks. While a pacemaker itself doesn't cause pain, the principle of choosing how one's end-of-life care proceeds is still very much in play. It's about respecting wishes, frankly.
This is a sensitive area, and discussions with the medical team are absolutely vital. They can explain what deactivation means for that particular patient and help families understand the process. It's about making informed choices during a very difficult time, you know, and having those conversations can bring a lot of comfort, really.
Who Performs Deactivation?
If the decision is made to turn off a pacemaker or other cardiac device, it's not something a family member can do on their own. This procedure is typically performed by a medical professional, often a cardiologist who specializes in heart rhythm issues. Sometimes, a representative from the pacemaker company itself might be involved, as they are very familiar with the specific device, basically.
These company representatives are usually available around the clock, with someone on call 24/7, to assist with these kinds of requests. The process itself is relatively simple, usually involving the use of a special magnet or programming device that communicates with the pacemaker. Essentially, the pacemaker has been chemically disconnected, or rather, its electrical output is stopped, so it no longer sends impulses to the heart, you know.
It's a quick and painless procedure for the patient, and it ensures that the deactivation is done safely and correctly. This is part of providing dignified care at the end of life, so it's important that qualified individuals handle it, actually.
What Happens to a Pacemaker After Death?
Once a person has passed away, the pacemaker stops having any effect on the body, as the heart muscle is no longer able to respond. However, the device itself is still inside the body. People often wonder what happens to it next. It's a practical question that comes up, you know, especially when making arrangements after a death.
Pacemakers and other implanted cardiac devices can be removed after a person's death. This is often done for a few reasons. One reason is that these devices contain batteries and other components that can be hazardous if cremated. So, for cremation, removal is usually a requirement, as a matter of fact. Another reason, which is really quite wonderful, is that these devices can sometimes be recycled for patients who cannot afford them. If you wish to do this, you should have a medical directive or discuss it with the funeral home, you know.
Since the person having the pacemaker removed is no longer living, there is no need for a doctor to remove the pacemaker after death. Either someone working in the hospital morgue or the mortician working at the funeral home you chose will be able to remove the pacemaker from your loved one’s body. This is a routine part of the post-mortem care in many places, so it's something that the funeral home can guide you through, really.
Safe management of pacemakers and other implanted devices needs careful consideration to ensure safe and appropriate care after death. This includes various types of implanted devices. It's a part of the dignified handling of a person's remains, so it's something that is well-established in practice, you know.
Frequently Asked Questions
Does a pacemaker prolong death when a patient is in last stages of death?
In general, pacemakers do not keep palliative care patients alive, as terminal events are often due to sepsis, hemorrhage, pulmonary emboli, or arrhythmias from metabolic issues. Most dying patients become acidotic before cardiac arrest, which effectively renders a pacemaker nonfunctional, as under such conditions, the myocardium does not respond to the pacemaker's discharges. Thus, for most patients, an active pacemaker will not affect the timing or circumstances of death. It may, very rarely, slightly prolong life, but this is not typical, you know.
Will a pacemaker keep someone alive after they die?
No, a pacemaker will not keep someone alive after they die. If the heart stops functioning due to other reasons, such as a lack of oxygen or a complete cessation of electrical activity, the pacemaker will no longer be effective, and the heart will stop. Once someone stops breathing, their body can no longer get oxygen, and the heart muscle will die and stop beating, even with a pacemaker. Therefore, the pacemaker does not prevent death or artificially keep the heart beating after someone passes away. You can stop worrying about your device keeping your body alive long after the rest of you leave this earthly existence, really.
Do you need to turn off a pacemaker after death?
No, you do not need to turn off a pacemaker after death for it to stop functioning. Once someone stops breathing, their body can no longer get oxygen, and the heart muscle will die and stop beating, even with a pacemaker. Therefore, the pacemaker will not prevent death and a patient will die from their terminal illness without turning off the pacemaker. However, pacemakers are often removed after death, especially if the body is to be cremated, or for recycling purposes. This removal is usually handled by hospital morgue staff or funeral home personnel, you know.
Understanding how does a pacemaker work when someone is dying can bring a lot of peace to families during a very tender time. It's about knowing that these devices are there to help with rhythm, but they don't override the natural course of life. For more information on heart health, you might want to explore resources like the American Heart Association, which offers a lot of helpful material. You can also learn more about cardiac care on our site, and we have more details about end-of-life planning here.
Detail Author:
- Name : Nicolette Smitham II
- Username : will.homenick
- Email : hegmann.alexane@cassin.biz
- Birthdate : 1973-01-10
- Address : 2104 Roxanne Spurs Greenholtshire, WA 21043
- Phone : 1-631-216-7174
- Company : Auer Inc
- Job : Power Distributors OR Dispatcher
- Bio : Sit illo sunt et qui iure. Dolore pariatur rem ut accusantium quod ea. Expedita beatae voluptatem nemo.
Socials
tiktok:
- url : https://tiktok.com/@cremina
- username : cremina
- bio : Et non at ipsam labore. Ratione deserunt eius et in. Quo soluta recusandae in.
- followers : 6748
- following : 1047
instagram:
- url : https://instagram.com/al.cremin
- username : al.cremin
- bio : Rerum eveniet omnis quibusdam autem impedit ipsa. Debitis accusantium aliquam molestias aut autem.
- followers : 1635
- following : 719
twitter:
- url : https://twitter.com/cremina
- username : cremina
- bio : Animi aut recusandae ullam qui. Vel nemo pariatur voluptates quod iste repellat.
- followers : 4231
- following : 411
linkedin:
- url : https://linkedin.com/in/al_cremin
- username : al_cremin
- bio : Odio quis impedit sunt voluptatem.
- followers : 2371
- following : 285